
Home
List your patent
My account
Help
Support us
Stereotactic Radiosurgery with SPECT/PET 3D Targeting
[Category : - HEALTH]
[Viewed 544 times]
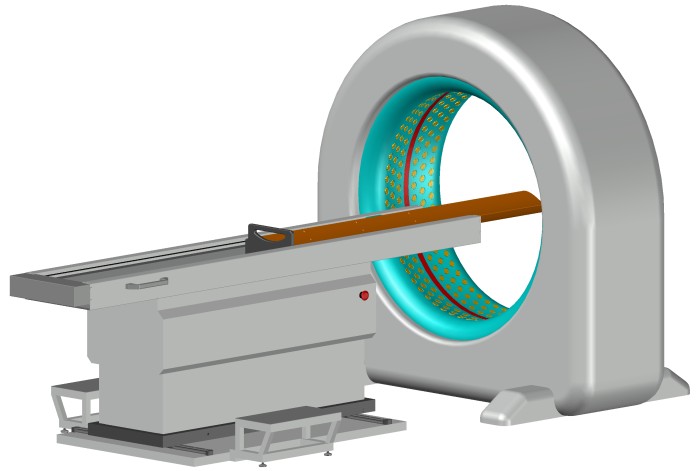
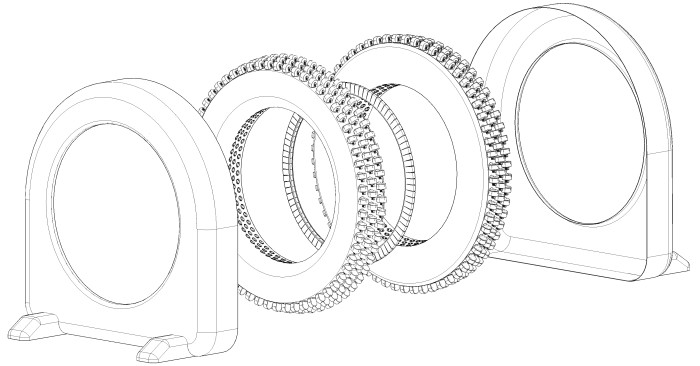
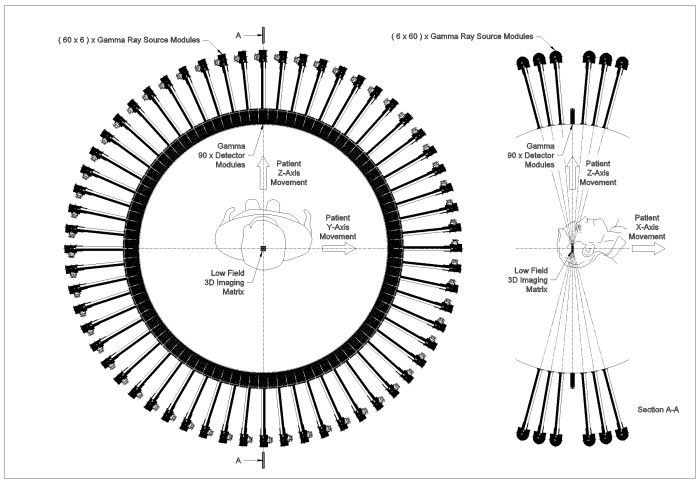
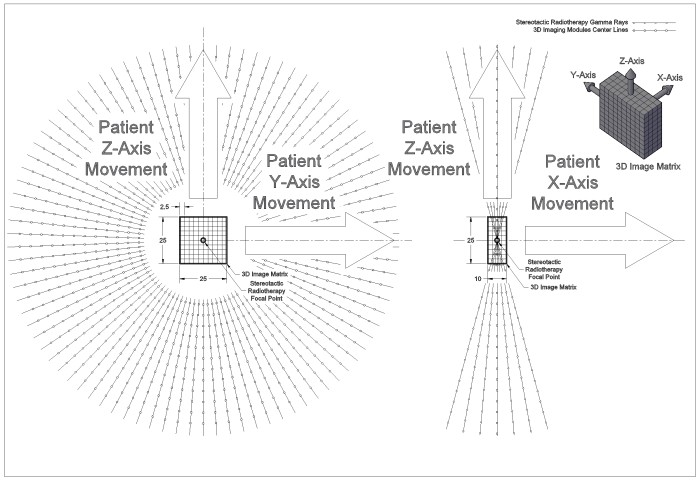
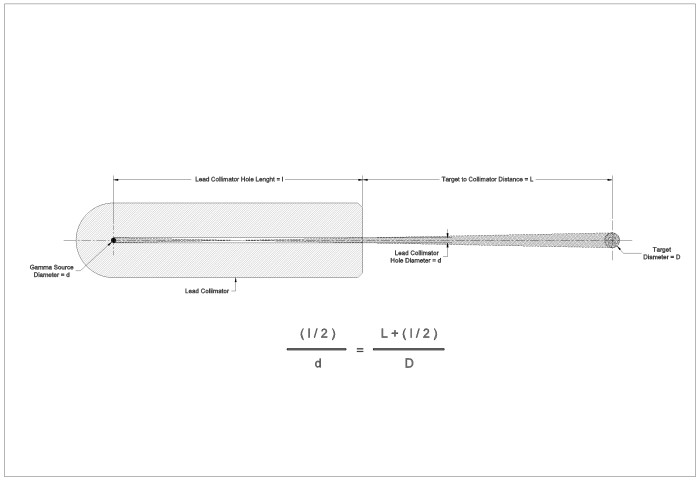
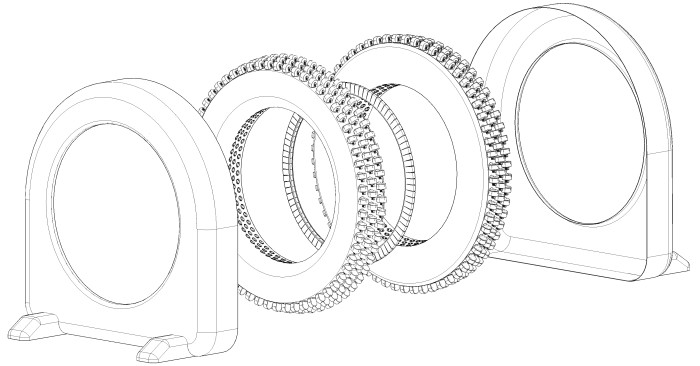
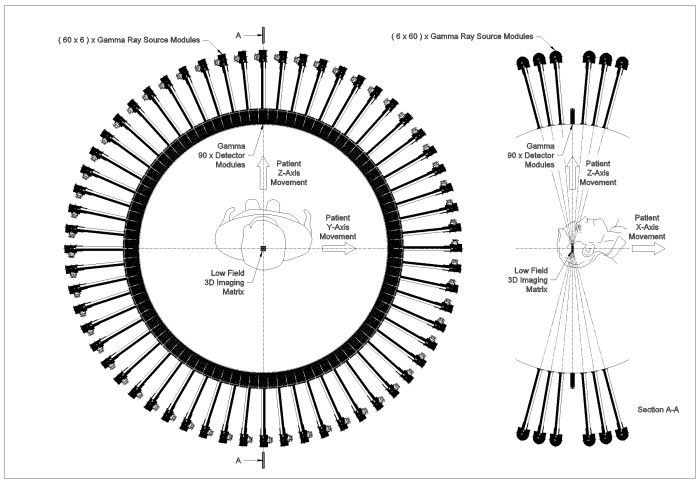
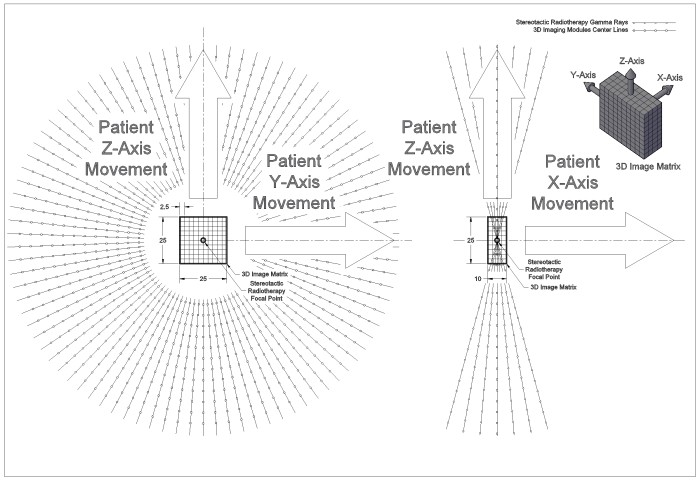
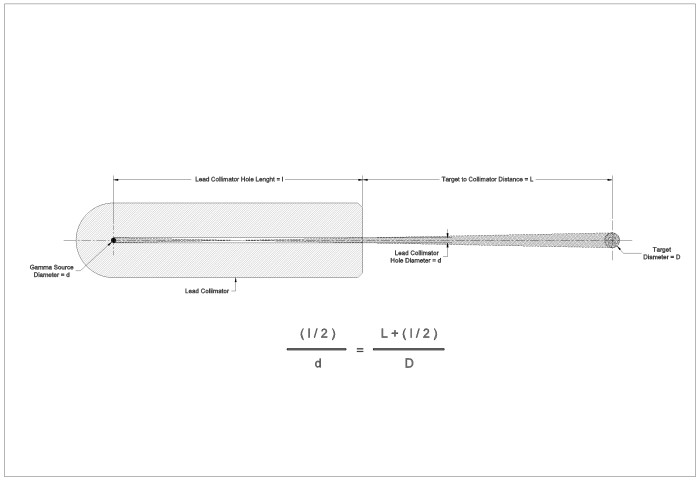
This is an integrated system, designed for use in the medical field, is employed in the treatment of various types of cancer. This is applicable in the treatment of all types of solid tumors, including but not limited to, brain, breast, cervix, larynx, lung, pancreas, prostate, skin, spinal cord, stomach, and uterine tumors, as well as soft tissue sarcoma and bone, leukemia, and lymphoma (tumors of the lymphatic system). It is also used in the treatment of some benign tumors. This system provides significant benefits including, but not limited to, integration of imaging and radiotherapy process, no need for stereotactic frames or other methods to determine tumor position in the simulation phase, and not causing stress and anxiety in the patient.rnCancer continues to be a leading cause of death worldwide. The treatment of this pervasive disease often involves the use of radiation therapy, a method that employs high-energy radiation to shrink tumors and kill cancer cells by damaging their DNA. However, traditional radiation therapy methods are associated with several limitations. Traditional radiation therapy may be invasive, causing significant stress and discomfort to the patient. The process may be physically and emotionally taxing, often leading to anxiety and decreased quality of life for the patient. Furthermore, these methods may not be applicable to all types of cancer tumors, limiting their effectiveness.rnAnother limitation of traditional radiation therapy is the separation of the diagnostic and treatment processes. The diagnosis of the tumor’s location, dimensions, and extent is often performed by 3D C.T Scan or MRI imaging systems separately from the radiation therapy (commonly known as simulation phase), leading to longer overall treatment times and increased discomfort for the patient. Since the diagnosis of the tumor’s location, dimensions, and extent of the tumor are performed on a separate device from the radiotherapy apparatus, physicians are required to use tools such as stereotactic frames in the Gamma Knife method, temporary or permanent tattoos, elastic meshes, plaster or foam molds to stabilize the patient’s body or organ and mark the location and extent of the tumor. This process can potentially cause significant stress and discomfort for the patient. The accuracy of targeting the tumor and avoiding nearby organs is another critical issue in traditional radiation therapy. Inaccurate targeting can lead to irradiation of healthy tissues and organs, leading to unnecessary side effects and complications.rnThe present system involves the integration of stereotactic radiosurgery with Single-Photon Emission Computed Tomography (SPECT) and/or Positron Emission Tomography (PET) for 3D targeting of cancerous tumors. This system aims to enhance the precision and effectiveness of radiation therapy while improving patient comfort and reducing treatment costs.rnMain Components:rnThe device in this invention comprises four main components that work simultaneously and interactively with each other:rna) The 3D imaging section using the PET or SPECT method, or a combination of both:rnThe primary objective of the 3D imaging section in this invention, which is essentially a radiotherapy device, is not to conduct a metabolic study or obtain a comprehensive image of the tumor. Instead, its function is to precisely locate the tumor, guide the radiotherapy section intelligently, and design an automatic and intelligent treatment plan. Therefore, the imaging section in this device has a small field of view. Naturally, the entire dimensions and extent of the cancerous tumor might not fall within the field of view of this imaging section. However, considering the role of this section in the overall radiotherapy process, this does not pose a problem; instead, it offers several advantages, which will be fully explored and detailed below. It is worth mentioning that gradually, during the radiotherapy process and by accumulating the small 3D images obtained, a complete 3D image of the tumor can eventually be achieved.rnThe output image from the imaging section is a small 3D image matrix. The dimensions of this 3D matrix are approximately X: 10.0 mm, Y: 25 mm, Z: 25 mm. It is important to note that these dimensions are provided as an initial reference and may change or be adjustable in practice. The geometric center of this rectangular cuboid-shaped matrix aligns with the center of the imaging system ring and also with the focal center of the stereotactic radiotherapy spherical sectors, which is the focal point of the gamma rays emitted from the gamma ray modules of the radiotherapy system.rnThe size of a 3D element (pixel) in this matrix depends on the final resolution of the imaging system. According to available data, the best conventional resolution for SPECT imaging devices is around 0.25 mm, and for PET imaging devices, it is about 0.75 mm; although, for radiotherapy purposes, a resolution of up to 2.5 mm is sufficient.rnAs mentioned above, the primary task of the imaging section in this invention is to locate cancerous tumors that have been tagged with appropriate radiopharmaceuticals, to guide and steer the radiotherapy system. To this end, the imaging section continuously and online provides a 3D matrix of the target area. Each element of this matrix, in addition to three-dimensional coordinates (X, Y, Z), has a fourth parameter called activity (A). The activity parameter actually indicates the amount of radiopharmaceutical uptake in that element. Since cancerous tumor cells, due to their higher activity and metabolism, absorb higher amounts of radiopharmaceuticals, they will have higher activity levels compared to healthy cells. Excessive activity in any element of the 3D image matrix indicates the presence of cancerous or potentially cancerous cells in that element. Additionally, the activity level in each cancerous element represents the number of cancer cells in that element. Therefore, elements with higher activity must be treated with higher doses. In the stereotactic method, the radiotherapy dose can be varied and adjusted by changing the number of gamma ray sources and the duration of gamma ray exposure. Hence, the imaging section provides a continuous and online 3D matrix image, indicating the status of the cells in the target point of radiotherapy (the focal center of the gamma rays emitted from the gamma ray modules of the radiotherapy system) and the surrounding cells, in terms of being healthy or cancerous, to the main control system of the device. The main control system uses this information as a roadmap to guide the stereotactic radiotherapy section. In other words, the main control system automatically and intelligently designs and predicts the path of the radiotherapy section in subsequent stages based on the information obtained from the imaging section.rnb) Stereotactic Radiotherapy Section Using Gamma Rays Emitted from Cobalt-60:rnThe radiotherapy section in this invention uses gamma rays emitted from cobalt-60 sources. Cobalt-60 can be obtained in the form of rods with various diameters and lengths. Cobalt-60 is the most common isotope used in radiotherapy and is a source of gamma rays with two notable energies, 1.33 MeV and 1.77 MeV, with a half-life of over 5 years.rnNote: Iridium isotopes are also used in radiotherapy devices, and if needed, this invention can use this isotope in a completely similar manner.rnThe use of cobalt-60 and gamma rays in radiotherapy compared to linear accelerators, which are sources of X-rays with various powers, has the following advantages:rn1. Simpler and More Reliable Mechanism: The mechanism and structure of the device, in terms of mechanics, electronics, and control system, are much simpler and more reliable compared to linear accelerators.rn2. Cost-Effective: The initial investment cost, maintenance, and repair expenses are significantly lower and more cost-effective compared to linear accelerators.rn3. Increased Dose at the Focal Point: It enables the use of multiple gamma ray beams for stereotactic radiotherapy, which increases the dose at the radiotherapy focal point and reduces the treatment duration.rnIn this invention, 360 gamma ray modules are used for stereotactic radiotherapy. However, this number can be adjusted to be fewer or more. These 360 gamma ray modules are located on two segments of a sphere with a diameter of 1200 millimeters. Each of these two segments is positioned on one side of the imaging ring. Each segment contains 180 gamma ray modules arranged in three rows of 60 each. In each row, 60 gamma ray modules are positioned at equal angular intervals. The gamma ray beam emitted from each module passes precisely through the center of the spherical segment, which coincides with the geometric center of the 3D imaging matrix.rnEach of the two spherical segments is made of aluminum. The inner diameter of these spherical segments is about 1200 mm, and the outer diameter is about 1800 mm. Each spherical segment has 180 holes for installing the gamma ray modules. The gamma ray source part of each module is installed on the outer side, and the collimator part of each module is installed on the inner side of the spherical segment. Each radiotherapy module is equipped with lead protective shields to prevent unwanted gamma ray leakage. The cobalt-60 rod is housed within a lead shield piece that can rotate relative to its fixed outer sheath by a small servo motor. This allows the gamma ray beam emitted from each module to be turned on and off as needed according to the radiotherapy program.rnWith this arrangement, the central control system, based on the images of the cancerous tumor provided by the imaging section, as well as the position of the tumor and the surrounding healthy and sensitive tissues, can activate a specific and necessary number of gamma ray modules. This ensures that the required dose is delivered to the target point of the cancerous tumor from the appropriate and desired angles for radiotherapy.rnEach gamma-ray module consists of two parts:rn1. Gamma-ray sourcern2. CollimatorrnThe cobalt-60 rod emits gamma rays in all directions, similar to a light bulb. The collimator's function is to parallelize the gamma rays emitted from the cobalt-60 rod and direct them towards the focal point of stereotactic radiotherapy. In other words, the collimator allows parallel and aligned rays to pass by eliminating non-parallel rays. By adjusting two parameters, the diameter of the collimator's lead shield hole and its length, the diameter of the gamma radiation circle at a specific distance can be controlled.rnrnIn this invention, collimators of equal length but with different hole diameters are used. These collimators come in three different sizes with irradiation area diameters of 2.5 mm, 4 mm, and 6 mm. Typically, a radiotherapy device equipped with this invention has several collimators of each size installed. On average, approximately 60% of the collimators can be chosen with a size of 2.5 mm, 20% with a size of 4 mm, and the remaining 20% with a size of 6 mm. However, these percentages can be fully adjusted based on specific needs. Based on the three-dimensional images obtained from the imaging section, the central control system for executing stereotactic radiotherapy selects an array of collimators with suitable irradiation area diameters to achieve the best radiotherapy results with the highest efficiency, maximum dose for cancer cells, and minimal dose for surrounding healthy cells.rnc) Patient positioning bed with linear movement along the three coordinate axes (X, Y, Z).rnThe device of this invention is equipped with a special bed for positioning the patient and guiding them into the radiotherapy device. This bed can move along the three coordinate axes (X, Y, Z) to place the patient in the desired position and coordinates or move them at pre-determined speeds. The bed, where the patient lies, is made of carbon fiber to ensure maximum mechanical strength, minimum thickness, and consequently, minimal absorption, attenuation, and scattering of gamma rays. This applies to both the gamma rays emitted from the radiopharmaceuticals used for imaging and the gamma rays emitted from the gamma-ray modules used for radiotherapy.rnSince no metallic or non-metallic part with a high gamma-ray attenuation coefficient can be located in the field of view of the imaging or radiotherapy system, the length of the bed in this device is designed so that any part of the patient's body affected by cancer can be positioned at the center of the imaging and radiotherapy ring. If multiple parts of the patient's body are affected by cancer (e.g., in metastasis conditions), it may be necessary to change the patient's position on the bed, and radiotherapy would be performed separately for each part.rnd) Central Control System:rn The central control system features an independent and high-speed computer. It receives the reconstructed three-dimensional images from the imaging section's computer and, based on these images, automatically and online, plans and executes the treatment program. The control system also manages the guidance and positioning of the device's bed.rnUsing the received images and following predetermined algorithms tailored for radiotherapy of each organ and body part, the central control system devises the treatment plan. It identifies cancerous elements within each three-dimensional imaging matrix and, according to existing algorithms, decides the direction and dose of gamma rays needed to irradiate the tumor. To this end, the system commands the relevant gamma-ray modules to activate and emit gamma rays. Depending on the tumor's extent, the control system might use gamma-ray modules with collimators of varying hole diameters.rnThe central control system determines the appropriate radiation dose by considering the tumor's location, the surrounding sensitive organs, and the activity level of the element within the three-dimensional matrix located at the focal point of radiotherapy, which indicates the malignancy of the cells in that element. The suitable dose is determined by selecting the number of gamma-ray modules, the appropriate angle, and the necessary irradiation duration.rnHow It Works:rnThe radiotherapist uses previous diagnostic imaging, which may be obtained through methods such as CT Scan, MRI, PET, or SPECT, to determine the approximate location of the tumor or cancerous tumors.rnDepending on the type of tumor to be treated, the appropriate radiopharmaceutical is injected into the patient, and a waiting period is observed for the radiopharmaceutical to be absorbed by the cancer cells of the tumor. This duration varies based on the type of radiopharmaceutical used. Subsequently, the patient lies on the treatment table of the radiotherapy system and is positioned appropriately for radiotherapy by the radiotherapist. Depending on the location and type of tumor, the patient may be placed on the table in a supine (face-up) or prone (face-down) position.rnIf necessary, the radiotherapist may use auxiliary tools and fixtures, specifically designed for this purpose, to stabilize the part of the patient’s body where the tumor is located. However, due to the operational method of this device, complete stabilization of the patient's body is not required. The radiotherapist ensures that the patient is completely relaxed in terms of their positioning on the table and their mental and emotional state, without imposing stress or anxiety on them.rnThen, the radiotherapist uses the three movement axes of the table to guide the patient towards the radiotherapy section, aiming to place the approximate location of the cancerous tumor at the center of the radiotherapy ring. The radiotherapist then leaves the radiotherapy room and issues the command to start the radiotherapy from the control room.rnBefore initiating the radiotherapy process, the radiotherapist must determine and set the imaging system protocol (SPECT/PET or combined) based on the type of radiopharmaceutical used. Additionally, the radiotherapist must select one of the appropriate treatment programs, considering the type and location of the cancerous tumor in the patient’s body. These predefined treatment programs are available in the system control software and can be customized with various adjustable parameters for each patient. Each treatment program includes predetermined and set parameters for stereotactic radiotherapy angles and other related parameters, based on the type of tumor, its location, and the surrounding sensitive tissues and organs.rnWith the start of the radiotherapy process, the imaging system begins to work according to the selected protocol (SPECT, PET, or combined). The imaging computer generates a small 3D image in a three-dimensional matrix format in each imaging cycle (e.g., every 15 seconds). This 3D image, once completed and processed, is sent to the radiotherapy computer.rnThe radiotherapy computer examines and reprocesses each 3D image matrix. If excessive activity is detected at the current position of the table and in the center of the 3D image matrix, indicating the presence of cancer cells in that element, the radiotherapy computer activates specific gamma ray modules based on the preselected program and the activity level of that element to perform gamma irradiation. In the stereotactic radiotherapy method, the dose emitted by each gamma ray module alone is not lethal to either cancerous or healthy cells. However, the convergence of multiple gamma rays, which reinforce each other at the center of the radiotherapy ring, creates a high, lethal dose for the cancer cells located in that area, leading to the destruction of their DNA strands and their subsequent death. If adjacent elements to the central element in the image matrix also exhibit high activity, the radiotherapy control system uses gamma ray modules with a larger irradiation area to irradiate a larger volume of the tumor at once, thereby reducing the radiotherapy duration.rnIf none of the elements in the 3D image matrix contain cancer cells, or if the central element does not contain cancer cells but other elements in the matrix do, the radiotherapy control system moves the table in appropriate directions to locate the cancer cells, position them at the focal center of the gamma ray modules, and carry out the radiotherapy process. The radiotherapy control system effectively scans the area where the radiotherapist has roughly identified the tumor’s location, automatically performing the radiotherapy process by detecting the cancer cells according to the predetermined treatment plan.rnThe scanning process to locate the cancer cells in this invention can be somewhat likened to the manufacturing process of parts in 3D printers. The control system scans the specified area layer by layer, and upon finding cancer cells or cells prone to becoming cancerous, targets them with lethal doses of gamma rays. In contrast, other radiotherapy methods rely solely on simulation phase data to approximate the tumor’s position relative to existing signs and references, assuming accurate targeting for radiotherapy execution.rnTherefore, because this invention continuously locates cancer cells with the help of real-time imaging during radiotherapy, any slight movement of the patient due to fatigue, stress, etc., is detectable in the 3D images taken. The radiotherapy control system will automatically make the necessary adjustments to compensate. Thus, this system eliminates the need for stereotactic frames and other harsh, stressful methods for tumor localization, allowing the patient to undergo treatment comfortably, calmly, and with minimal stress.rnAs the radiotherapy process progresses and the suspicious area for the presence of a cancerous tumor is fully scanned, the imaging system can provide a precise three-dimensional image of the shape and tissue of the tumor undergoing radiotherapy. This information can be used to evaluate the treatment course and the effectiveness of the radiotherapy in subsequent treatment stages.rnThe control system in the radiotherapy device of this invention also calculates and considers the cumulative gamma radiation dose received by each element. For example, an element that is not located at the center of the 3D image matrix might receive a non-effective dose during a radiotherapy session due to being in the path of a gamma ray beam. It is possible that the same element could again be in the path of another gamma ray beam during the radiotherapy of another cancerous element and receive another non-effective dose. The device's control system, using the three-dimensional coordinates of the treated area and considering the executed treatment plan, is capable of calculating the cumulative dose for each element in the radiotherapy field. This information helps ensure that the control system applies an appropriate dose to the cancerous cells while preventing damage to adjacent healthy cells and tissues.rnAdvantages of the This Invention Compared to Prior Devices: rn1- **Simultaneous Tumor Positioning and Radiotherapy**: In the radiotherapy device of this invention, the process of determining the position, dimensions, and extent of the tumor is performed simultaneously with the radiotherapy process. Therefore, there is no need to install a stereotactic frame or other similar auxiliary equipment on the patient's body to determine the position, dimensions, and extent of the tumor. This ensures that the treatment with this device brings the least stress and anxiety to the patient, providing comfort and ease during the treatment stages.rn2- **Comprehensive Treatment Method**: This invention offers a comprehensive method for treating most cancerous tumors that can be marked with radiopharmaceuticals.rn3- **Reduced Treatment Time**: The integration of the processes of determining the position, dimensions, and extent of the tumor with the radiotherapy process in this invention reduces the treatment time, making the treatment process easier for the patient and providing greater comfort.rn4- **Fewer Radiotherapy Sessions**: Utilizing the stereotactic irradiation method with a concentrated dose at a very small point within a sphere diameter of 1 to 2.5 millimeters in this invention reduces the number of radiotherapy sessions.rn5- **Increased Targeting Accuracy**: The integration of the processes of determining the position, dimensions, and extent of the tumor with the radiotherapy process in this invention increases the accuracy of targeting the cancerous tumor, avoiding irradiation of adjacent organs and tissues.rn6- **Controlled Gamma Radiation Sources**: In this device, each gamma radiation source can be controlled to turn on and off by the control system. This allows for variable dose irradiation during the scanning of the cancerous tumor online, according to the activity level of the tumor at that point.rn7- **Reduced Costs**: Treatment costs, initial investment, operating costs, maintenance expenses, and operator costs of this device are significantly reduced due to the integration of the processes of determining the position, dimensions, and extent of the tumor with the radiotherapy process and the simplification of the device's working mechanism.rn8- **Intelligent Treatment Planning**: Given the integration of the processes of determining the position, dimensions, and extent of the tumor with the radiotherapy process, it is possible to design an automatic and intelligent treatment plan online, based on the simultaneous imaging results of the cancerous tumor in this device.rn9- **Minimized Human Error**: Due to the working method of the device in this invention, human errors resulting from designing incorrect, inaccurate, and unprincipled treatment plans will be greatly reduced.rn10- **Claustrophobia-Friendly Design**: Since the radiotherapy section of this invention has a very large internal diameter (approximately 1200 millimeters), patients with claustrophobia will not experience fear and anxiety during treatment with this device.rn11- **Enhanced Penetration Power**: The system in this invention uses gamma radiation for radiotherapy, which has more energy and penetration power compared to devices using X-rays. Therefore, this allows the system to effectively and efficiently treat most cancerous tumors throughout the body, even those located in deeper parts relative to the body's surface. rnrnNote 1: This invention has been registered on July 01, 2023 under patent application No. 140250140003002349 in the Intellectual Property and Patent Registration Department of Iran. rnrnNote 2: This invention has been filed on June 26, 2024 under No. PCT/IB2024/056187 in the World Intellectual Property Organization (WIPO).rn
 Patent publications:No publication
Patent publications:No publication
Asking price:
Make an offer
[ Home
| List a patent
| Manage your account
| F.A.Q.|Terms of use
| Contact us]
Copyright PatentAuction.com 2004-2017
Page created at 2025-12-17 1:43:19, Patent Auction Time.

 Patent publications:
Patent publications: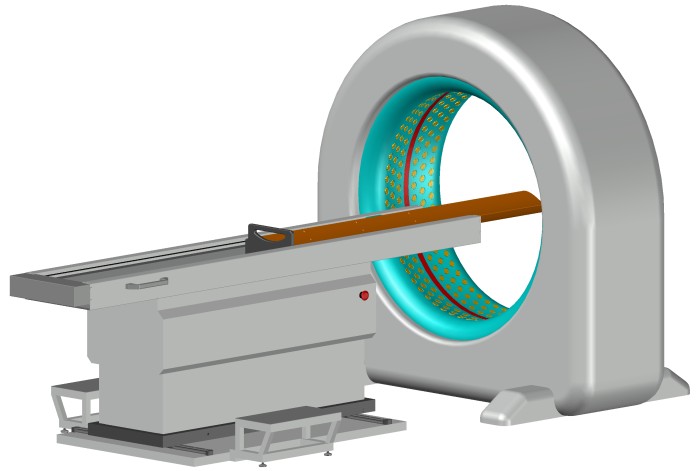
 Great invention
Great invention